Becoming a parent often brings the question: “When will my baby sleep through the night?” The reality is that breastfeeding and sleep do not always look like the neat schedules shown in books or online. Babies wake often, sometimes nurse for comfort as much as nutrition, and their sleep patterns shift as they grow. This is normal, and understanding what is expected when you breastfeed can help families cope with broken sleep and make nights more manageable.
Understanding Baby Sleep in the Early Weeks
Why newborn sleep looks different from adult sleep
Young babies and infants sleep in short cycles of two to three hours, with only a few hours at night before waking again. This lighter, more frequent sleep helps protect infants by reducing the risk of deep, prolonged sleep that can be unsafe. Waking often is a natural survival mechanism, not a sign something is wrong. This pattern is illustrated again in Healthy sleep for your baby and child, which notes that newborns may sleep up to 18 hours a day, often in stretches of 3 to 4 hours. As babies grow, their sleep gradually becomes more predictable, with longer stretches at night and more regular naps during the day.
How breastfeeding supports natural baby sleep patterns
Breastfeeding helps regulate a baby’s circadian rhythm. Breastmilk contains hormones like melatonin that change across the day and night, helping babies learn healthy sleep patterns. Breastfeeding provides closeness and warmth, easing babies into sleep in a way that matches their developmental needs.
Night Waking and Breastfeeding: What Parents Should Expect
Is it normal for my baby to wake so often at night?
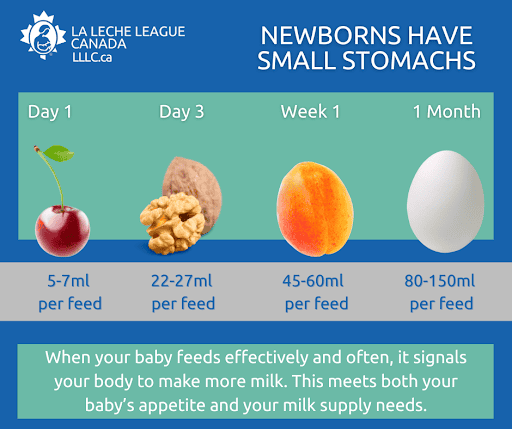
Yes, yes and yes, 100% so. At birth, the infant’s mouth takes over from the umbilical cord that was the constant source of nutrition and oxygen. The mouth becomes the avenue to feed the newborn now outside the uterus. The size of a newborn’s stomach, at birth, has a capacity to hold between 3-7 ml of colostrum (the first breast milk) at each feed. In fact, the colostrum has been found to smell and taste like amniotic fluid. The recognizable smell and taste for the baby outside the womb must be comforting, and is designed to be their first food. Babies practice swallowing in utero. The newborn stomach stretches gradually over the next week to a capacity of 1.5 to 2 ounces, up to about 60 mL, then more over the first month reaching a capacity of 80-150 mL or 3-5 ounces. The stretching of the newborn’s stomach coincides with the mother’s milk “coming in” and volume of milk increasing over the first week, and increased volumes with age.
Human breast milk is species-specific, and the components (except vitamin D) meet all of the infant’s nutritional requirements for their first 6 months of life. Breastmilk is digested and tolerated by newborns as intended to, and empties from their stomach in 2–3 hours, and then they need more. So they wake and ask to be fed. The point here is that the stomach will fill and empty frequently because it is.
Immediately following birth the following key elements can set the trajectory of the breastfeeding relationship, they are 1) Feed the baby, 2) Protect mother’s milk supply and 3) Keep Mother and baby together. When these elements are adhered to, the rest of the feeding journey into place. A baby who is in close proximity to their mom will be attended to when they show early signs of hunger, so can be offered their mom’s breast and will feed calmly. I always say the baby is THE BEST pump. Mom releases milk for her baby, and communication from the breast to the brain is best done by her baby. If any of these key elements are missing, things don’t go as they ought to. A separation due to maternal or infant medical needs puts a detour in the milk making plans. All is not lost and there is support for moms and baby’s that are separated following birth. This is when a pump is required to establish, build and maintain milk supply.
Why night feeds are important for growth and milk supply

Many parents wonder whether they should breastfeed at night, but these feeds are essential. The baby is asking to be fed. Night nursing stimulates milk production because prolactin, the milk-making hormone, is highest overnight. These feeds are especially important in the early weeks as your supply is being established. Responding to your baby’s night cues not only helps them grow but reassures them that their needs are met.
Comfort Nursing vs. Feeding: How to Tell the Difference
What comfort nursing is (and why it matters for babies)
Comfort nursing is when a baby latches for reassurance rather than hunger. It can look like shorter, fluttery sucking rather than strong, rhythmic feeding. This behaviour supports emotional regulation, reduces stress, and is a natural part of the breastfeeding relationship.
Signs your baby is feeding for hunger vs. comfort
- Hunger feeding: deeper, longer sucks and swallows, sustained for several minutes
- Comfort nursing: lighter, fluttery sucking, often with a sleepy baby
Both types are valuable. One meets nutritional needs, the other meets emotional and developmental needs. Feeding to sleep is not a bad habit. It is a normal and healthy way babies settle.
Safe Sleep and Breastfeeding: Making Nights Easier
Following the Safe Sleep Seven guidelines
The Safe Sleep Seven guidelines from La Leche League International explain when bedsharing can be made safer for breastfeeding families. They include factors such as the baby being full-term, breastfed, on a firm mattress, and parents avoiding smoking, alcohol, drugs, or unsafe bedding.
Bedsharing, room-sharing, and separate sleep surfaces
Some families choose to bedshare, others prefer a crib or bassinet near the bed. Room-sharing is recommended for at least the first 6 months, as it lowers the risk of sudden infant death syndrome and supports infants as they adjust to nighttime feeding and comfort needs. Always use a firm mattress and keep pillows, blankets, and other soft items away from your baby. See more baby sleep science research from BASIS. For further evidence-based recommendations, the Academy of Breastfeeding Medicine’s bedsharing protocol provides practical guidance.
Coping With Broken Sleep as a New Parent
Practical rest and naptime strategies for mothers
Many mothers struggle to get enough sleep. You may wonder how much sleep is enough, especially in the newborn stage. Short naps, dimming lights in the evening, and calm nighttime routines can help. Even small rest periods matter, and protecting maternal sleep improves both recovery and milk supply. Other mothers find that short naps or quiet rest breaks help them feel more restored.

How partners can help with nighttime breastfeeding

Partners play an important role. They can bring the baby for feeds, handle burping and diaper changes, and offer emotional support. Knowing you are not alone at night can reduce stress and make breastfeeding more sustainable. Gentle bedtime routine practices also help babies learn the difference between day and night without the need for formal sleep training.
Common Breastfeeding and Sleep Patterns Over Time
What changes after the newborn stage
As babies grow, sleep stretches often lengthen, but mothers should know that night waking can continue for months or even years. Teething, growth spurts, and developmental leaps can all lead to more frequent nursing at night. This is expected and usually temporary.
When to seek extra help if sleep or feeding feels hard
If you are struggling with exhaustion, sleep problems, pain during feeds, or concerns about your baby’s growth, reach out for support. A board-certified lactation consultant (IBCLC) can assess feeding, help with latch and positioning, and give advice tailored to your situation. According toCanada’s Breastfeeding Progress Report 2022, 91% of mothers initiate breastfeeding, but exclusivity declines in the first six months, showing how common challenges like sleep can affect feeding journeys.


