If you’re worried about low milk supply, you’re not alone. It’s one of the most common concerns new parents face when breastfeeding, especially during those early weeks filled with sleepless nights, constant baby feeding, and well-meaning advice from every direction.
So what’s our direction? Compassionate care grounded in evidence-based practice. That means as a Lactation Consultant we help cut through the noise to help you make the best possible decision for you and your baby, by offering real insight into breastfeeding and how to navigate concerns about not producing enough milk.
We’ll start by understanding how breast milk is produced — from milk ducts and breast stimulation, to the flow of milk and even the role of your baby’s skin. Then we’ll look at a common experience called Perceived Insufficient Milk (PIM), and why that might actually be a good sign. After that, we’ll explore clinical causes of low milk supply, which include physical and hormonal factors that affect milk production. Finally, we’ll walk through strategies to support your breastfeeding journey and what it looks like to bring everything together. We also understand that your body and your baby are changing as the time goes by, so what was applicable to a week old baby may not be the same for a baby who is a month old.
Understanding how your body produces milk for your baby is the first step in identifying what’s normal and when support might help.
How Milk Production Actually Works
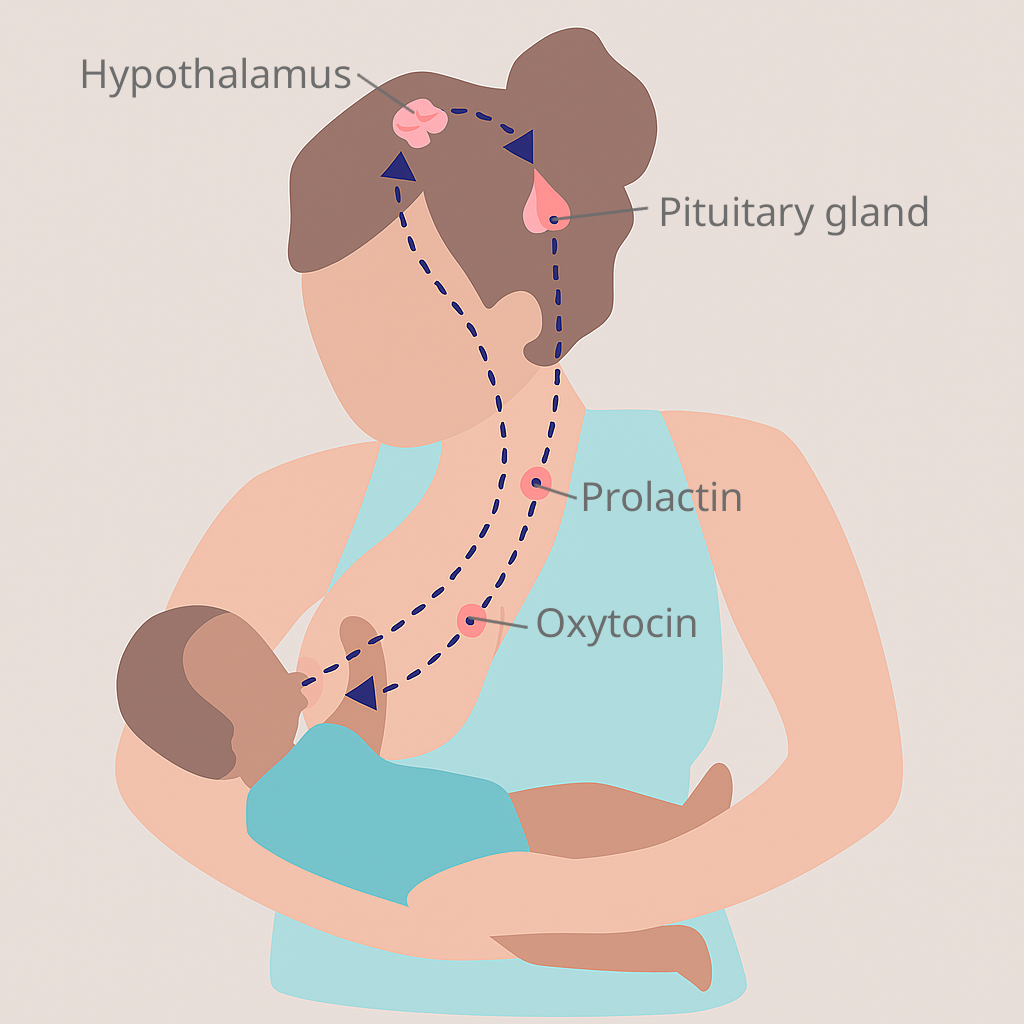
Technically, lactation involves the coordinated interaction of epithelial acini, ductal branching, and neuroendocrine reflexes originating in the hypothalamus and pituitary axis. If that made your eyes glaze over, you’re not alone. Thankfully, understanding the basics of how milk is made does not require a science degree.
Here’s what really matters.
Your Baby Sends the Signals, Your Body Does the Work
Lactation works through a feedback loop that is well understood biologically, but not always easy to navigate in real life. While the process relies on milk being removed from the breast to signal the body to make more, many mothers find that supply concerns, pain, or feeding challenges can make that loop feel anything but simple for producing enough milk.
When milk is removed from the breast ideally, by a baby’s direct latch and suckling, your body receives the strongest signal to make more. This is because the combination of touch, pressure from suckling, and oral stimulation activates multiple pathways for hormone release. In addition to you visualizing your baby, at your breast, both before and during their feeding. There are also feelings of contentment and happiness in doing what you intended to do during motherhood.
While hand expression and pumping can also help maintain and increase milk supply, nothing quite replaces the signals your body receives from your baby at your breast, I call the baby the best pump.
The process starts during pregnancy, kicks into high gear a few days after birth, and continues as long as milk keeps being removed regularly. It is dynamic and responsive, not fixed.
After birth, the expulsion of the placenta causes progesterone levels to drop. In response, the hormone prolactin spikes, thus supporting milk production. Oxytocin then helps with milk release, creating the feedback loop that powers ongoing lactation.
And in some cases, there may not have been a pregnancy . With the right combination of hormonal support and consistent stimulation, it’s possible to induce lactation without ever having been pregnant. This is often part of feeding plans for adoptive parents, surrogate situations, same sexcouples, or those in shared nursing relationships. While more complex to initiate, this shows just how adaptable the human body can be when it comes to nourishing a baby.
Fun fact: Some people have active milk ducts in their armpits. It’s called axillary breast tissue — a quirky reminder that our bodies are wired for flexibility.
Your Brain Is Part of the System Too
Milk supply is not only physical. Your emotions, stress levels, and mental well-being can all affect how milk flows while breastfeeding. The hormone oxytocin helps move milk through your ducts, but it also helps you feel calm and connected. If you are anxious, exhausted, or overstimulated, it may be harder to release milk even if your body has made enough.
That’s one of the reasons perceived low milk supply is so common. You can be doing everything right and still feel like something is off. Sometimes, the system is working just fine, but the signals or expectations don’t line up. We’ll unpack that next.
Understanding Perceived Low Milk Supply
You can be doing everything “right” and still worry that your baby isn’t getting enough milk. That doesn’t mean your body isn’t working. It means the system is more complex than people realize — and most mothers haven’t been shown or been exposed to what normal looks like.
This experience is known as Perceived Insufficient Milk (PIM). It’s when your milk supply is actually fine, but your baby’s behavior, your expectations, or the stress of it all makes you question that. This is not just in your head, it’s a very real, and very common, concern.
What Makes Mothers Think They Have Low Milk Production?

Even in healthy breastfeeding relationships, signs like fussiness, frequent feeding, or shorter feeds can seem like red flags. But most of these are within the normal realm of human babies behavior:
- Babies breast feed often, especially at night, because human milk digests human milk efficiently, usually by 2-3 hours..
- Feeds may be short or long,both are normal.They can range from 5-40 minutes, but on average are 20 minutes.
- Crying or restlessness doesn’t always mean hunger. Your baby is communicating with you, perhaps they have a wet or dirty diaper, perhaps they are lonely and want to be entertained.
- Soft breasts or not feeling full or leaking does not mean you’re not producing milk. Most lactating breasts become softer around 2 weeks, not always the overfull feeling like they had during the first 1-2 weeks.
- Social media, schedules, and outdated advice can create pressure to follow feeding patterns that don’t reflect human biology or normal infant behavior.
- Sudden increases in nursing frequency are often growth caused by a growth spurt, not signs of not having enough breast milk. These natural phases help your baby signal your body to make more milk and typically pass in a few days.
Most of these signs are misread because our culture has moved away from showing what normal breastfeeding looks like. When you haven’t grown up seeing babies breastfeed, it’s easy to think something is wrong with supply when your baby doesn’t fit a tidy routine.
How confidence and culture shape our perception
Perceived low breast-milk supply is often rooted in how disconnected modern life is from shared, community-based learning. Instead of watching aunties, sisters, or friends breastfeed, we scroll through apps and advice threads. These often don’t match reality.
Mental health plays a big role too into the amount of milk produced. Anxiety, exhaustion, or postpartum depression can make it harder to read your baby’s cues, and harder to trust yourself. It’s an understandable reaction to doing something hard without enough support. Over time you get to know your baby and what their subtle and more pronounced cues are signaling. You know your baby best.
When well-meaning friends or family say things like “they must still be hungry,” it can start to feel like you’re doing something wrong. But remember: many of these beliefs were shaped during a time when alternative feeding methods were marketed as modern and scientific. That’s not your fault — and it’s not your family’s fault either. It’s the result of a couple of generations of commercial messaging that replaced traditional breastmilk intake with convenience.
A Note on Compassion and Support
We understand how personal this topic is. Doubt, guilt, or even shame can surface, especially if feeding hasn’t gone the way you hoped. Using alternative feeding methods, following an assessment and a feeding plan to get on track, does not make you a bad parent, it means you are doing what you think is best given the circumstances. A care plan that truly supports you should reflect your choices, your baby’s needs, and the reality of your current situation. Care plans are usually a temporary plan that is continually re-evaluated, and updated as feeding progresses.
Research shows that feeding decisions are often tied to complex emotions. Parents who use alternative methods may feel judged or second-guessed by others, while breastfeeding parents can struggle with pressure to “do it right,” or discomfort around public or prolonged feeding. These feelings don’t mean you’ve done anything wrong, they reflect a culture that often makes feeding harder than it needs to be.
At Feed and Thrive, we are guided by two core beliefs:
- We will always feed the baby, and feeding with confidence is essential. That means understanding the recommendations necessary at that time, not being shamed by them.
- You deserve support that’s evidence-based and rooted in care, not guilt or pressure.
This is your feeding journey. Our job is to help you navigate it with clarity and compassion.
What Can Actually Cause Low Milk Supply?
If you’ve already ruled out latch issues, babies feeding patterns, and common misunderstandings, it’s time to look at the real possible causes: your milk supply might be low. True low milk supply is much less common than it feels, but when it does happen, there’s almost always other causes, and often, a way forward.
Sometimes it’s medical, sometimes it’s technical, and sometimes it’s a combination of events.. This isn’t about fault or failure. It’s about getting the full picture so you can get the right kind of help.
Physical or hormonal factors that affect milk production
Some medical conditions can make it harder for your body to produce enough milk, especially in the early weeks:

- Retained placenta or heavy blood loss after birth can delay or disrupt the hormonal shift that triggers milk production.
- Polycystic ovary syndrome (PCOS), thyroid disorders, diabetes, and other hormonal imbalances may interfere with supply. This doesn’t mean you can’t breastfeed — it just means you might need extra support.
- Insufficient glandular tissue (IGT), often tied to how the breasts developed during puberty, can limit how much milk is produced, though it’s more rare than often assumed.
- Breast surgery or injury can impact nerves and ducts involved in milk flow, depending on the type and location.
- Physical separation from your baby such as when your baby is admitted to the Neonatal Intensive Care Unit (NICU), or when you require treatment in an Intensive Care Unit (ICU) after birth—can delay or disrupt the establishment of breastfeeding.
If any of these apply to you, it doesn’t mean breastfeeding isn’t possible. It means it’s worth working with someone who understands how to navigate reduced milk production challenges safely.
Feeding patterns that interfere with milk supply
Even if your body can make enough milk, certain routines can disrupt the feedback loop that keeps it going:
- Scheduled feeds instead of feeding on demand can signal the body to slow down production.
- Long gaps between feeds, especially at night, may cause a gradual drop in supply.
- Poor milk removal from shallow latch, tongue or lip ties, or weak sucking means the breast isn’t being drained adequately, which will decrease milk supply over time.
- Bottle preference or early pacifier use can also impact how often baby cues to breastfeed.
These issues often fly under the radar because they look like normal baby behavior. A baby who fusses or seems full after a short feed may not be getting what they need, even if it seems like they are.
Other factors and medications that may play a role
- Certain medications or hormonal birth control, especially those containing estrogen, can reduce milk supply in some people.
- Chronic stress, sleep deprivation, or postpartum mood disorders can affect hormone levels and milk let-down. These don’t mean you’re not trying hard enough. They mean you need support, not pressure.
- Supplementing early or unnecessarily can cause your body to miss signals to produce more milk, which then makes supplementing feel even more necessary.
If any of this sounds familiar, it doesn’t mean you’re stuck. It means you’re closer to understanding what your body needs and how to work with it.
How to Increase Milk Supply Safely and Effectively
When there is a true drop in milk supply, there’s almost always a reason. And more importantly, there are often ways to improve it. That doesn’t mean doing everything perfectly or turning feeding into a full-time job just to get a full milk supply. It means understanding your body’s milk production process and knowing when to ask for support.
These strategies focus on the basics first, then build from there. Not every tip will be right for every family, but they can help you choose your next step with clarity and confidence.
Breastfeeding more often and remove more milk
Breast milk production is driven by demand. The more milk your baby removes through feeding, the stronger the signal to your body to produce more. A breast pump can help support this process, but nothing stimulates supply quite like a well-latched baby.
- Offer the breast frequently, even if baby just fed. Many babies “snack” during growth spurts or cluster feeding periods.
- Don’t limit time at the breast. Let baby finish fully on one side before switching.
- If baby is skipping feeds or not removing much milk, consider adding a pumping session after or between feeds to increase stimulation.
Make sure baby is nursing well
Even frequent feeds won’t help if milk isn’t being removed effectively. This often comes down to latch, position, or oral anatomy.
- Look for wide, deep latches with good jaw movement and audible swallows.
- If nursing is painful or baby slides off often, a tongue tie check or position adjustment may help.
- Try laid-back or body-led positions to allow baby’s instincts to guide feeding.
A lactation consultant can help identify these issues quickly — often in just one session.
Use pumping to support (not replace) breastfeeding
Pumping can help boost milk output when baby isn’t feeding efficiently or if extra breast milk needs to be stored. But pumping alone doesn’t always send the same hormonal signals as a baby at the breast.
- Pump after feeds to increase output, especially in the morning when milk production is often higher.
- Use hands-on pumping or breast compressions to increase flow.
- Double pump for 10–15 minutes if skipping a feeding.
Don’t stress over ounces. Many people produce more milk with baby than with a pump. It’s normal for milk supply to fluctuate throughout the day.

Spend more time skin-to-skin
Skin-to-skin is not just for bonding. Baby skin helps regulate their systems and supports the hormones responsible for let-down and ongoing milk production.
- Rest baby on your bare chest during naps or calm, alert periods.
- Let baby nuzzle and root at the breast to stimulate natural feeding cues.
This is especially helpful during growth spurts or any dips in milk supply.
Focus on nourishment and rest
Your body makes breast milk by drawing on your own energy and nutrient stores. No single food or tea guarantees results, but consistent care of your body makes a big difference.
- Eat balanced meals and drink to thirst. Undereating or strict diets can impact overall milk supply.
- Focus on protein, healthy fats, and complex carbohydrates over processed foods.
- Rest when you can, even if it’s a short nap. Sleep and emotional well-being are tied to healthy lactation and hormonal balance.
Stress, burnout, and fatigue can all impact milk production. You matter in this process too.
What about galactagogues and supplements?
Some herbal remedies and foods are marketed as ways to increase breast milk. While a few may support the body, they should never replace frequent feeding or proper support.
- Fenugreek, goat’s rue, and blessed thistle are commonly used but not for everyone.
- Always speak with a care provider before using galactagogues, especially if you have health conditions or are on medication.
No supplement can overcome a problem with milk removal — and that’s always the first place to start.
When supplementation is needed
In some cases, even after doing everything right, breast milk supply remains low. This doesn’t mean breastfeeding must stop. It means your plan may include more tools.
Supplementation can happen in a way that still protects your nursing relationship. This may include:
- Expressed breast milk
- Donor milk from a screened, regulated source
- In rare cases, other feeding methods that are used with care
Using tools like a supplemental nursing system (SNS) or paced bottle feeding can help keep baby at the breast while still meeting their full nutritional needs.
If alternative feeding becomes part of your plan, that’s okay. Your efforts and your relationship with your baby are still valid and important. Support can help you combine feeding methods without sacrificing connection or confidence.
Why Getting Help Can Change Everything
If you’ve tried these steps and still feel stuck about having low supply, you are not failing. Your baby is not broken. Your body is not broken. It simply means you deserve more support.
So many factors shape your feeding experience. How much time off you have, whether you’re working from home, how soon you’re expected to return to work, how much sleep you’re getting, and what kind of help you have around you. All of it matters. And it can make something that is already challenging feel even harder.
That is why we do not just share information about milk supply. We offer care that fits your real life. One-on-one breastfeeding support can bring clarity when nothing else seems to help. Not because you are doing something wrong, but because sometimes a conversation and a care plan built around your needs is exactly what makes the difference.
If you are not sure what to do next, reach out. You do not have to figure this out alone.


